Allogeneic hematopoietic stem cell transplantation (allo-HCT) is a cornerstone of curative therapy for patients with high-risk hematologic malignancies. For practicing hematologists/oncologists, optimizing the pathway and timeline from diagnosis to transplant is critical — not only for outcomes but also for patient experience. Traditionally, patients with acute leukemia are first treated by a leukemia specialist to achieve remission and only later referred to a transplant expert. This fragmented model can lead to duplicative conversations, mixed messages, and delays that sometimes necessitate additional "bridging" chemotherapies before transplant.
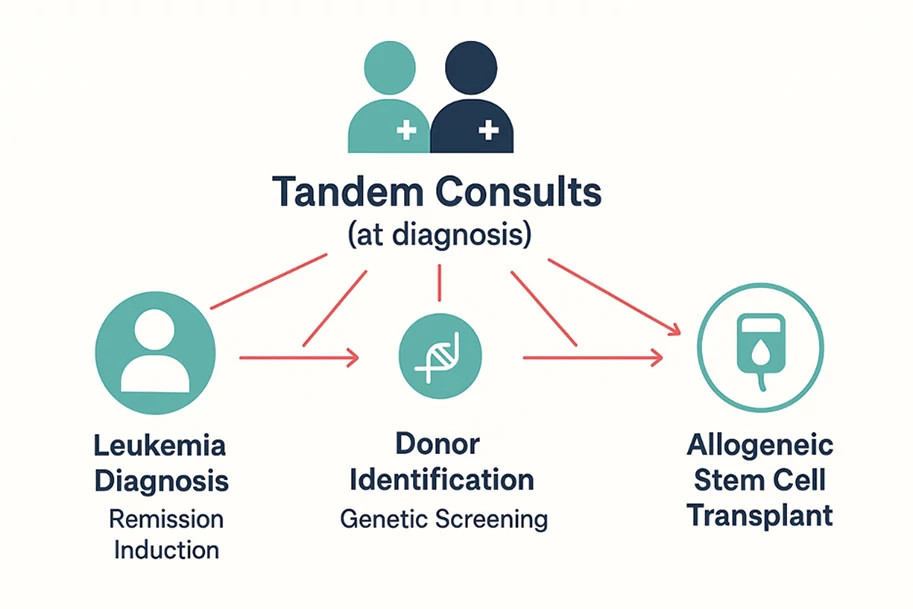
To address these challenges, we developed a tandem leukemia/stem cell transplant consult model at Dana-Farber, in which patients with newly diagnosed or relapsed leukemia are evaluated simultaneously by a leukemia specialist and a transplant physician at their initial visit. This approach promotes early alignment of treatment strategy, facilitates patient education, and streamlines transplant planning — critical for patients who may require time-sensitive interventions.
Integrated Evaluation from Day One
During the tandem consult, patients know from the outset that they are cared for by a team of leukemia and transplant physicians working in constant communication. Together, they review diagnostic findings; cytogenetic and molecular reports; measurable residual disease (MRD) status; and prior responses to define a personalized plan and timeline. This shared encounter allows both providers to contribute expertise in real time — establishing transplant eligibility, identifying potential medical or lifestyle barriers, and crafting a unified plan that balances remission goals with optimal timing for allo-HCT.
The model also facilitates early risk-benefit discussions. Adverse genomic features or suboptimal MRD clearance may not only shape pre-transplant therapy but also influence the urgency of donor identification. Patients and families benefit from a single, coordinated message about prognosis and next steps, reducing confusion that can arise when discussions occur separately.
Pre-Transplant Therapy
With few exceptions, patients with acute leukemia require some form of induction therapy to reduce disease burden before transplant. Tandem consults allow leukemia and transplant physicians to collaboratively define the best approach — whether it includes intensive chemotherapy, reduced-intensity regimens, targeted agents (e.g., FLT3, IDH inhibitors), or clinical trials.
Input from the transplant physician is crucial, since induction therapy can influence transplant timing, donor search urgency, and conditioning intensity. For example, patients treated with intensive chemotherapy may need an earlier transplant, while those receiving reduced-intensity regimens may have more time for donor identification. This co-management ensures that treatment intensity, timing, and toxicities are aligned with patient performance status, disease features, and transplant goals.
Early Donor Selection and Planning
The tandem model accelerates HLA typing and donor identification. Patients receive immediate counseling on donor options — matched or mismatched related/unrelated donors, haploidentical family donors, or umbilical cord blood — framed within their disease kinetics and transplant urgency. In some cases, early donor identification can even influence therapeutic choices.
Importantly, patients with blood cancers may carry germline genetic variants predisposing them to leukemia. Detecting such variants early allows physicians to screen or defer related donors, ensuring safe donor selection. Coordinated planning between leukemia and transplant specialists enables this rapid and thoughtful approach.
Multidisciplinary Support and Care Continuity
Tandem consults are supported by transplant nurse coordinators, pharmacists, social workers, and fertility preservation specialists. Addressing psychosocial, logistical, and financial issues early helps prevent delays and improves patient experience across the treatment continuum.
For referring hematologists, the model ensures patients receive well-coordinated care and a clearly articulated plan. By integrating transplant planning into the initial consultation, we provide a streamlined, patient-centered approach that aligns all stakeholders around a common goal: moving patients toward curative therapy with efficiency and clarity.