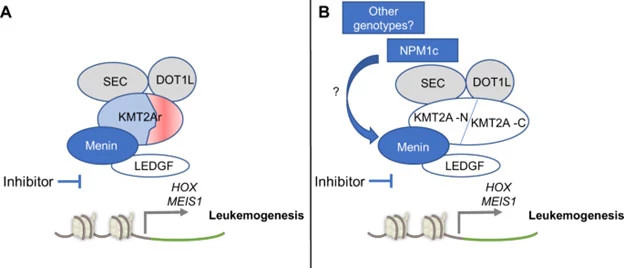
A new and potentially broadly applicable class of anti-leukemic agents has arrived on the scene due to preclinical work done in the laboratory of Scott Armstrong, MD, PhD, of Dana-Farber Cancer Institute in collaboration with members of the Adult Leukemia Program within Medical Oncology at Dana-Farber led by Richard Stone, MD, Chief of Staff. The laboratory science suggested that a sizable percentage of patients with acute myeloid leukemia (AML) as well as acute lymphoblastic leukemia (ALL) develop leukemia due to changes in regulation of gene expression caused by an abnormal transcriptional complex, an amalgamation of proteins that directs transcription of certain genes which promote leukemia. This transcriptional complex includes a small protein called menin, which is altered in leukemia patients whose blasts have a KMT2A rearrangement or point mutation in NPM1.
Until Dr. Armstrong’s work, it was not possible to envision drugs that disrupted a protein-protein complex to downregulate transcription of leukemogenic genes. However, drugs in this class displace menin and eradicate this disease when fed to laboratory animals with specific model leukemias. This exciting finding in the preclinical studies was replicated in a trial known as Augment-101 (Dana-Farber 19-467; NCI 04065399) performed in relapsed and refractory KMT2A rearranged and NPM1 acute leukemia patients using the first-in-class menin inhibitor (revumenib). The oral revumenib was particularly active in leukemias which harbored KMT2A rearrangements, which tend to be more common in younger adults and children, such that the FDA granted approval for this agent in relapsed/refractory KMT2A rearranged AML in the fall of 2024 and in relapsed/refractory NPM1 mutated AML on October 24, 2025. The menin inhibitors, similar to retinoic acid therapy in acute promyelocytic leukemia can lead to differentiation syndrome, a potentially dangerous side effect. Differentiation syndrome is readily managed by holding drugs and giving steroids. Revumenib is otherwise well-tolerated with side effects including myelosuppression and QT interval prolongation.
Evidencing the potential success of menin inhibitor therapy in AML, there are many other drugs in this class which are being tested, including bleximenib, also the subject of a clinical trial (Dana-Farber 21-355; NCI 04811560) in advanced patients with similar types of AML here at Dana-Farber. Most exciting is the eventual utility of these agents in combination with standard chemotherapy in newly diagnosed older and younger adults and children with leukemias dependent on this transcriptional machinery. Another trial soon to start at Dana-Farber (Dana-Farber 24-747; NCI 06852222) will test whether or not the addition of bleximenib to the typical initial chemotherapy given to older adults with AML (azacitidine and venetoclax – the latter being another drug developed here by Anthony Letai, MD, PhD, and Jacqueline Garcia, MD, PhD) will improve the outcome of older adults who generally receive this non-intensive chemotherapy backbone. This type of trial would not have happened without close collaboration from scientists like Drs. Armstrong and Letai, along with clinicians such as Drs. Stone and Garcia and many other members of the Adult Leukemia Program.
The ultimate goal of this research is to develop personalized medicine that enables an individual with acute leukemia, formerly treated with cytotoxic chemotherapy, to receive all-oral therapy associated with minimal side effects. This is yet another example of Dana-Farber’s involvement in the development of new drugs in cancer generally and in leukemia specifically. The Adult Leukemia Program in the Department of Medical Oncology at Dana-Farber has played a role in preclinical and/or clinical testing of many recently approved agents including midostaurin, asciminib, inovsidenib, enasidenib, venetoclax, tagraxofusp, avapritinib, inotuzumab, and blinatumomab.